Reports of deaths potentially linked to the treatment have cast a shadow on what many hail as a landmark approval.
The US Food and Drug Administration (FDA) has approved lecanemab, the second-ever treatment for Alzheimer’s disease intended to tackle the root of the condition and slow cognitive decline. Researchers welcome the decision, but the excitement is clouded by patient deaths and reports that the FDA acted improperly when approving the first such drug last year.
By slowing progression of the disease when taken in the early stages of Alzheimer’s, lecanemab will allow individuals to have “more time to participate in daily life and live independently”, says Joanne Pike, president and chief executive of the Alzheimer’s Association in Washington DC, in a statement.
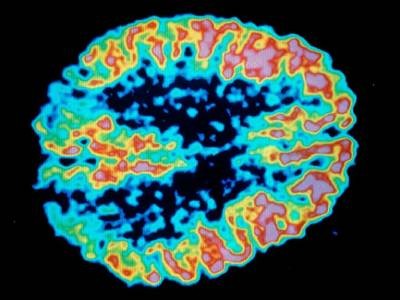
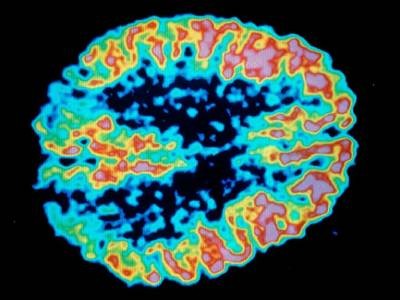
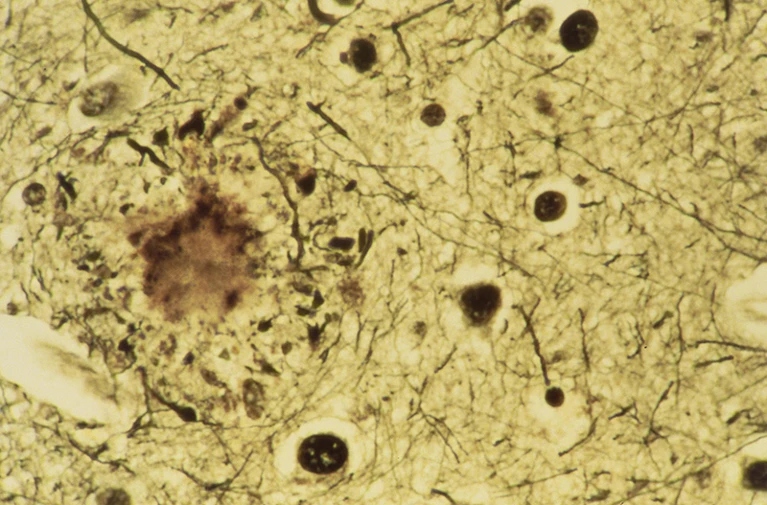
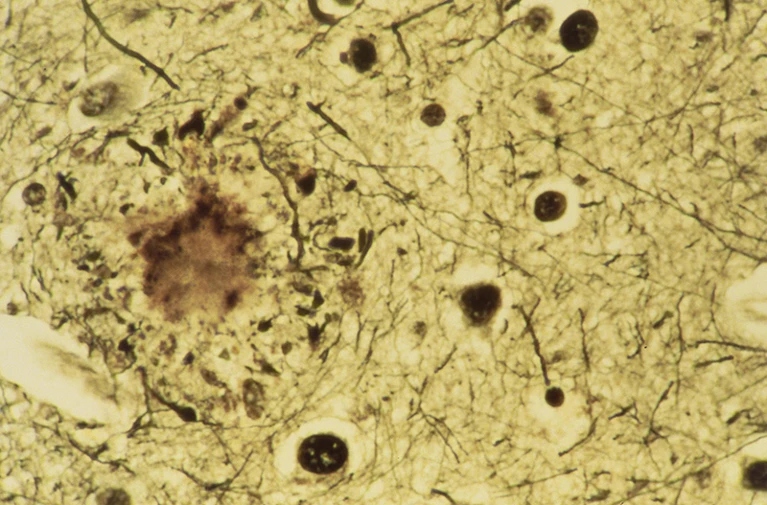
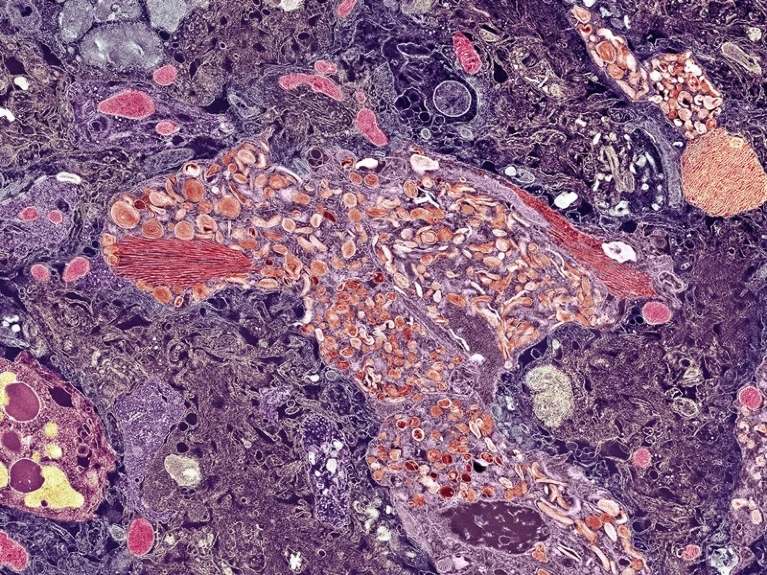
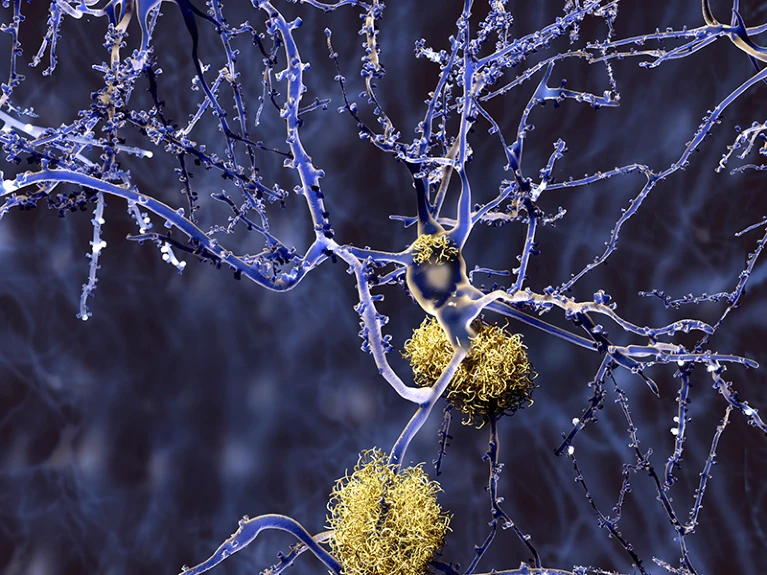
Lecanemab, which will be sold under the brand name Leqembi, is the first Alzheimer’s treatment to slow cognitive decline in a robust clinical trial and the second to be approved in less than two years. It is made by the biopharmaceutical companies Eisai, in Tokyo, Japan, and Biogen in Cambridge, Massachusetts. The drug, a monoclonal antibody, is intravenously infused into patients, enters the brain and clears the amyloid plaques believed to cause cognitive impairment and dementia in Alzheimer’s.
“The findings provide hope for patients and families, but it is also an important step in the development of successful ways to modify and prevent the clinical onset of the disease,” says Eric Reiman, executive director of the Banner Alzheimer’s Institute in Phoenix, Arizona.
By slowing progression of the disease when taken in the early stages of Alzheimer’s, lecanemab will allow individuals to have “more time to participate in daily life and live independently”, says Joanne Pike, president and chief executive of the Alzheimer’s Association in Washington DC, in a statement.
Lecanemab, which will be sold under the brand name Leqembi, is the first Alzheimer’s treatment to slow cognitive decline in a robust clinical trial and the second to be approved in less than two years. It is made by the biopharmaceutical companies Eisai, in Tokyo, Japan, and Biogen in Cambridge, Massachusetts. The drug, a monoclonal antibody, is intravenously infused into patients, enters the brain and clears the amyloid plaques believed to cause cognitive impairment and dementia in Alzheimer’s.
“The findings provide hope for patients and families, but it is also an important step in the development of successful ways to modify and prevent the clinical onset of the disease,” says Eric Reiman, executive director of the Banner Alzheimer’s Institute in Phoenix, Arizona.
Unclear impact
Lecanemab was authorized under the agency’s ‘accelerated approval’ pathway, which is reserved for therapies for diseases that have few treatments; it also does not require phase III clinical trial data. But researchers are hopeful about Biogen and Eisai’s phase III data, which were published in November 20221. That trial, conducted in about 1,800 people with early-stage Alzheimer’s, found that the antibody slowed cognitive decline by 27% over 18 months of treatment.
The FDA’s decision does not take the phase III study into account — Biogen and Eisai asked for accelerated approval on the basis of phase II data, which they submitted before the latest trial results were announced. The phase II study found that lecanemab decreased plaques in the brains of 856 patients, but did not assess whether this affected patients’ cognitive abilities. This is the same pathway used to approve its predecessor, aducanumab, a similar antibody also made by Biogen and Eisai.
It’s unclear what impact that 27% effect will have on the lives of people with Alzheimer’s — or whether that effect will persist after 18 months. It could mean, Reiman says, “an extra 6 months of recognizing a loved one’s face, or performing a valued activity”. But that will require future research, he says. In the meantime, the FDA says, lecanemab is to be used only for people with mild cognitive impairment — the same cohort as in the clinical trials.
The FDA’s decision does not take the phase III study into account — Biogen and Eisai asked for accelerated approval on the basis of phase II data, which they submitted before the latest trial results were announced. The phase II study found that lecanemab decreased plaques in the brains of 856 patients, but did not assess whether this affected patients’ cognitive abilities. This is the same pathway used to approve its predecessor, aducanumab, a similar antibody also made by Biogen and Eisai.
It’s unclear what impact that 27% effect will have on the lives of people with Alzheimer’s — or whether that effect will persist after 18 months. It could mean, Reiman says, “an extra 6 months of recognizing a loved one’s face, or performing a valued activity”. But that will require future research, he says. In the meantime, the FDA says, lecanemab is to be used only for people with mild cognitive impairment — the same cohort as in the clinical trials.
Treatment risks
Diana Zuckerman, president of the National Center for Health Research, a non-profit organization in Washington DC, isn’t sure that the benefit will be worth the risk. “You’re dealing with people with mild cognitive impairment who are functioning, and you’re putting them at risk,” both in terms of their health and finances, she says. Eisai says that a year of lecanemab will cost US$26,500 in the United States.
In recent months, Science and STAT News reported three people who had been enrolled in the lecanemab phase III study and then died during the extended phase of the trial, when patients receiving placebo can ask to be given the drug. They died from complications involving brain bleeding and seizures. According to those reports, researchers think that the patients might have died because of a set of conditions known as amyloid-related imaging abnormalities (ARIA). They suspect the antibody weakened blood vessels in the brain as it attacked the amyloid plaques lining them. All the patients were taking anticoagulant drugs at the time, which may have worsened the bleeding.
Eisai has said that it is inappropriate to draw conclusions on the basis of individual cases, and that it reported the deaths to the FDA as required. Nevertheless, the FDA’s approval requires that lecanemab include a warning about ARIA, and that physicians monitor for the condition, which it says is rarely serious or life-threatening.
The controversy around aducanumab, which the FDA granted accelerated approval on 7 June 2021, has cast a shadow over lecanemab. Many researchers thought that aducanumab, which also goes by the brand name Aduhelm, did not show a strong signal of cognitive decline. The FDA’s own scientific advisory panel recommended against approving the antibody in an 8–1 vote, and three panel members resigned after the FDA authorized it anyway. The FDA did not hold a public advisory meeting for lecanemab before approving it.
In recent months, Science and STAT News reported three people who had been enrolled in the lecanemab phase III study and then died during the extended phase of the trial, when patients receiving placebo can ask to be given the drug. They died from complications involving brain bleeding and seizures. According to those reports, researchers think that the patients might have died because of a set of conditions known as amyloid-related imaging abnormalities (ARIA). They suspect the antibody weakened blood vessels in the brain as it attacked the amyloid plaques lining them. All the patients were taking anticoagulant drugs at the time, which may have worsened the bleeding.
Eisai has said that it is inappropriate to draw conclusions on the basis of individual cases, and that it reported the deaths to the FDA as required. Nevertheless, the FDA’s approval requires that lecanemab include a warning about ARIA, and that physicians monitor for the condition, which it says is rarely serious or life-threatening.
The controversy around aducanumab, which the FDA granted accelerated approval on 7 June 2021, has cast a shadow over lecanemab. Many researchers thought that aducanumab, which also goes by the brand name Aduhelm, did not show a strong signal of cognitive decline. The FDA’s own scientific advisory panel recommended against approving the antibody in an 8–1 vote, and three panel members resigned after the FDA authorized it anyway. The FDA did not hold a public advisory meeting for lecanemab before approving it.
In aducanumab’s shadow
Since aducanumab’s approval, Biogen and the FDA have come under further scrutiny that has limited the treatment’s rollout. A congressional investigation released last month found that the agency had flouted its own rules by improperly guiding Biogen through the aducanumab approval process. The report said that the process was “rife with irregularities” and raised “serious concerns about FDA’s lapses in protocol and Biogen’s disregard of efficacy”, but does not impose any penalty on the FDA or the companies.

The US Center for Medicare and Medicaid Services (CMS) has declined to cover aducanumab under federal insurance plans unless a person is enrolled in a clinical trial, leaving most patients to pay over $28,000 for a year of treatment. CMS — and several clinics that refused to prescribe the drug — cited its questionable efficacy, drawing the ire of advocacy groups who say it should be readily available.
Despite the controversies, Reiman hopes that lecanemab’s success will open the door to more accelerated approvals in the future. He is currently partnering with pharmaceutical company Eli Lilly to test its similar monoclonal antibody, donanemab, in a phase III trial that he says is promising so far. The FDA is expected to decide whether to approve donanemab in the coming weeks.

The US Center for Medicare and Medicaid Services (CMS) has declined to cover aducanumab under federal insurance plans unless a person is enrolled in a clinical trial, leaving most patients to pay over $28,000 for a year of treatment. CMS — and several clinics that refused to prescribe the drug — cited its questionable efficacy, drawing the ire of advocacy groups who say it should be readily available.
Despite the controversies, Reiman hopes that lecanemab’s success will open the door to more accelerated approvals in the future. He is currently partnering with pharmaceutical company Eli Lilly to test its similar monoclonal antibody, donanemab, in a phase III trial that he says is promising so far. The FDA is expected to decide whether to approve donanemab in the coming weeks.



 January 10, 2023
January 10, 2023 By admin
By admin